The Role of CBT (Cognitive Behavioural Therapy) in Treating Depression
By Dr. Gillian Moore-Groarke, Chartered Health Psychologist
Introduction
For the past eighteen years working as a psychologist in a clinical setting depression is by far the most common presenting problem in my rooms. Depression presents in several different forms and generally requires a multi-disciplinary approach to treatment. There are many various triggers for depression. Unfortunately, some sufferers are born with neurological disorders that leave them pre-disposed to depression. However, for most suffers depression occurs as a result of adapting to changing life events which can be extremely stressful and generally the sufferer is at a loss to use appropriate coping mechanisms. Depression presents a significant challenge for ‘mind over mood’, Greenberger & Padensky 1995.
Psychiatrists and general practitioners prescribe various anti-depressant medications to people who are depressed. However, there are certain patients who prefer not to take medication but this is very much dependant on how debilitating the depression is for the patient. Sometimes I feel a patient may need to be on medication before they can engage psychologically but the preference is always to limit medication as much as possible due to various side effects.
I have been fortunate to work with psychiatrists and general practitioners that share my viewpoint of limiting medication as much as possible but being practical at the same time. (Moore-Groarke 2008) Medication is also not recommended for pregnant women or nursing mothers.
What is depression and what factors are important in depression
The DSM IV suggests that between 10-25% of women and 5-12% of men will experience depression at some stage in their lives. The predominant symptomatology of depression includes depressed mood and poor motivation levels and interest in one’s daily activities. Secondly symptomatology includes fatigue, increase or decrease in appetite, fitful and disturbed sleeping patterns, diminished concentration, an obvious reduction in self-esteem with recurrent ideation regarding death and suicide. It is the varying degrees of such symptoms that dictate the degree of depression present in the patient.
Beck’s (1976) etiological theory of depression suggests that depression relates to an underlying shift in a person’s cognitive perception of his world. Usually the person experiences a deep sense of loss which impacts greatly on his personal life. There are many varying degrees of loss e.g. loss of health, loss of youth –by growing old, loss of professional status or promotion, loss of a relationship through death, separation or divorce. Of course we can also be influenced by anticipatory loss e.g. fear of loss in the future e.g. loss of one’s job, partner, success, financial security and so on.
Beck’s theory states that depressed people think the way they do because their thinking is based towards negative interpretations of the world. According to his theory, depressed people acquire a negative ‘Schema’ of the world in childhood and adolescence as an effect of stressful life events. When the person with negative ‘Schemata’ encounters a situation that in some way resembles the conditions in which the original schema was learned, the previous negative schemata of that person are activated. Seligman in (2002) refers to these phenomena as ‘Learned helplessness’.
However, when we try to put depression in context, the onset of the illness of depression and the course it takes is significantly impacted by the environment the patient finds themselves in.
Carr in 2006 believes a family history of depression is a significant predisposing factor. Other important factors include childhood adversity, poor parental care, and loss of a parent. Low levels of sunlight also contribute to what we know as Seasonal Affective Depression (S.A.D. syndrome) and many sufferers of S.A.D. only take medication during the long, dark winter months and find that they improve greatly once the amount of sunlight increase. Segal et al (2002) made the point that depression is likely to reoccur again at stressful periods in one’s life e.g. loss of a family member or even a minor setback. Prior history of depression therefore increases vulnerability in the future. The trick here of course is to teach a patient to identify the triggers as quickly as possible once symptoms begin to appear.
A stressful environment is one of the most significant maintenance factors in depression, hence treatment programmes must be vigilant in teaching a sufferer of depression how to manage their stress. Relaxation therapy combined with stress/coping skills is useful. I also encourage patients to engage in regular exercise as part of their treatment. Expanding social connectedness and opening up opportunities for new interaction with people helps people overcome loneliness and isolation. Good social support systems help reduce or even break the cycle of depression.
History of Cognitive Behavioural Therapy
The roots of CBT can be traced back to the development of behaviour therapy in the early Twentieth Century. The development of cognitive therapy in the 1960’s, and the subsequent merging of the two. Initially the work focused on many of the neurotic disorders and it had little success in treating depression.
However, behaviourism was losing its popularity due to the so called ‘cognitive revolution’. The therapeutic approaches of Beck and Ellis gained popularity. Inspired by Ellis Aaron T. Beck developed cognitive therapy in the 1960’s. During the 1980’s and 1990’s cognitive and behavioural techniques merged together into CBT as we know it today.
Arnold Lazarus expanded the scope of CBT to include physical sensations (as distinct from emotional states), visual images (as distinct from language-based thinking) interpersonal relationships and biological factors.
What is CBT
Beck (1976) cognitive model the cognitive triad is composed of the following.
- A negative view of the world in general.
- A person’s negative view of themselves.
- A negative view of the future.
This cognitive triad affects interconnected components of our emotional, motivational, cognitive, behavioural and physiological well-being.
Ellis in (1987) had his own version of the triad. Depression he said was a maladaptive cognitive shift and he suggested the main agents of depression were as follows:
- A devout belief in one’s own personal inadequacy.
- The ‘horror’ of not having what one needs.
- The ‘awfulness’ of the way our live seems.
Given the general agreement around the cognitive shift model of depression by all the major CBT players put simply.
It is a way of thinking about, how you think about yourself, the world and other people, how what you do affects your thoughts and feelings.
CBT can help you to change how you think (cognitive) and what you do (behaviour). There changes can help you to feel better. Unlike some of the other therapeutic approaches it focuses on the ‘here and now’ problems and difficulties. Instead of focusing on the causes of your distress or symptoms in the past (just as in a psychotherapeutic approach), it looks for ways to improve your state of mind now.
It has been found helpful in anxiety, panic, agoraphobia and other phobias, social phobia, eating disorders, OCD (obsessive compulsive disorder) PTSD (post-traumatic stress disorder), schizophrenia as well as depression.
The basic model can be formulated as follows.
- A= Activating Agent – something of perceived personal importance has happened in the person’s environment.
- B = Belief – the activating agent has been filtered through a deeply held belief and has caused an evaluated response. – This belief triggers a negative automatic thought.
- C = Consequential behaviour by evaluating A and B the person will learn to adopt (what they see as) an appropriate response behaviour.
A useful way to help a patient to distance themselves from their NATs (negative automatic thoughts) is through the use of a Daily thought record.
The parts of this record are as follows:
- Thoughts
- Emotions
- Physical feelings
- Actions
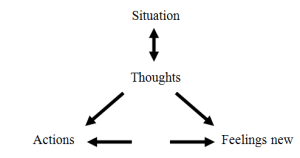
How you think about a problem can affect how you feel emotionally and physically. It can also alter what you do about it. There are many helpful and unhelpful ways of reacting to most situations, depending on how you think about them.
For example:
Jim is a very hypersensitive 20 year old. He reacts badly to lots of situations and engages in very extreme negative thinking patterns. This has always been the way until he entered therapy. For years he blamed his childhood, his dysfunctional family etc… but using cognitive behavioural therapy has encouraged him to play a proactive role in his own recovery. Here is an example of his Daily Thoughts record.
Situation: Jim is walking down town. He is feeling bad and even to get out to the shop to buy bread and milk is a chore. His old friend John walks by and apparently ignores him.
| Unhelpful | Helpful | |
| Thoughts | John ignored me- it’s obvious he doesn’t like me or have time for me anymore | Maybe he is wrapped up in his own troubles- something could be upsetting him |
| Emotional feelings | Depressed, sad, rejected, low | Concerned for the other person |
| Physical | Nauseous, crampy, lethargic | None – I feel ok |
| Action | Rush home – avoid him in future | Maybe get in touch, check in to see if he is alright. |
As you can see from this example the same situation has led to two very difficult results depending on how you think about the situation. Your thoughts affect your feelings which in turn effect what action you take.
If you retain the negative thought process you are likely to go home brooding over what happened and feeling worse. If you make the effort to get in touch with the other person you’ll feel better about yourself. This is summarised in the following ‘5 areas diagram’.
Cognitive distortions
A useful addition to the Daily thoughts record is the Cognitive Distortion list. This list outlines a number of common cognitive distortions that many sufferers of depression exhibit. Some common patterns of negative and irrational automatic thoughts include: (Moore-Groarke 2005)
- Catastrophizing – always anticipating the worst possible outcome to occur (e.g. I will be on the list of people to be let go from work).
- Filtering – exaggerating the negative and minimizing the positive aspects of an experience (e.g. focusing on all I had to do to get the extra financial reward, rather than enjoying the benefits of the extra monetary gain).
- Personalizing – automatically accepting blame when something bad occurs even when you had nothing to do with the cause of the negative event (e.g. he didn’t make contact because he must see me as boring).
- (Over) Generalising – Viewing isolated trouble events as evidence that all events to follow will be troubled, (e.g. if at the start of the holiday I am depressed, I will be depressed for the entire holiday).
- Black or white/polarized thinking – no middle ground or shades of grey (e.g. I missed one exam question therefore I’m useless, stupid, instead of I did pretty ok. Anyway).
- Emotionalizing – allowing feelings about an event to override logical evaluation of the events that occurred during the event (e.g. I feel so stupid that it is obvious I am a stupid person).
Dysfunctional beliefs are learned thinking habits that have no rational basis. Because such beliefs are not linked to reality very well, they tend to appear distorted. Despite such a high level of distortion, dysfunctional beliefs are all people typically have to help them make sense out of stressful events that they experience. Cognitive appraisals or snap judgements based on assumptions present within dysfunctional beliefs end up being biased and irrational. When people look to these appraisals of stressful situations to know how to react they regularly see the situation as simply awful.
They react to that false or exaggerated sense of awfulness and invariably experience strong depressive symptomatology.
Assumptions and core beliefs
Core beliefs are fundamental assumptions people have made that influence how they view the world and themselves. People get so used to thinking in these core ways that they stop noticing them or questioning them. Simply put, core beliefs are the unquestioned background themes that govern depressed peoples’ perceptions (e.g. a depressed person might think ‘I am inadequate’, ‘I am inferior’, because these beliefs are unquestioned, they are acted upon as though they are real and true.
Core beliefs serve as a filter through which people see the world. They influence the development of ‘intermediate beliefs’ which are related attitudes, rules and assumptions that follow from core beliefs.
One way to identify assumptions and core beliefs is to look for recurring themes in the daily thoughts records completed. If certain types of automatic thoughts repeatedly occur, they may provide a clue to your assumptions and core beliefs.
e.g. Common themes include fear of failure, feelings of inferiority, poor self-esteem, lack of confidence, not being good enough etc…
A second way to identify core beliefs is called the downward arrow technique. This technique is where you take a negative thought and you ask the question what does it mean about you until you eventually get to the core belief.
e.g. John does think Mary likes him (what’s so bad, or what does this mean?)
![]()
When I get close to someone, they end up disliking me? (what does this say about John?)
![]()
I’ll never have a close relationship (what does this say about John)
![]()
I’m unlikeable (This is his core belief – this is how John sees himself)
Activity Scheduling
Other exercises can be completed listing evidence to support or refute negative thoughts and this will help towards activity scheduling to map out homework assignments.
Homework assignments are the means by which the client gets to practice the more functional behavioural strategies identified during the session. Depressed people typically adopt an attitude that tasks will be too hard and even if they complete them there will be no personal reward or gain.
Example of activity and goal setting
| Goal | Try to develop a positive attitude regarding getting up early, even though I find the mornings difficult. |
| Action plan | Start day with relaxation exercise before getting out of bed. Eat breakfast with the family. Take your time. |
| Time to begin | Today |
| Possible obstacles to achieving goal | I can’t relax when the family are in and out and there is ware to be put into dishwasher, and tidy up. Everybody doesn’t sit down at the same time. |
| Strategies to overcome obstacles | Set table at night. Agree a time for all family to be at breakfast table. |
| Progress Report | Jan. 8th, Couldn’t relax. Jan 10th, organising the table helped, I could relax over breakfast. Jan. 12th, Despite the mess we all had breakfast at 8am |
During therapy it is useful to ask the client to rate the degree of difficulty and the degree of pleasure they anticipate from completing a piece of homework. Very often the client is surprised when they realise the task wasn’t as difficult as they had previously thought.
All the exercises discussed in the chapter are very beneficial in challenging the negative depressed disposition of the client. Of course the list is not exhaustive but I have tried to cover the most frequently used techniques. I also find the use of the Beck Depression Inventory or other Psychologists use the Burns Depression Checklist to evaluate a patient’s progress throughout the therapy (usually once a month).
What does the session involve?
Cognitive behavioural therapy can be done individually or with a group of people. I predominantly work with a patient individually although for relapse prevention sessions or workshops I work in groups of 4 to 6 patients.
Session number varies from 5-20 or more sessions depending on the severity of the problem. Each session lasts 30 minutes, some patients prefer a 60 minute session and this is often beneficial in the early stages of therapy when a patient is acquiring the skills of cognitive behavioural therapy.
In the first 2 to 4 sessions, it is important for me to check that the patient is comfortable with the type of treatment and that the patient agrees to do the homework exercises. Sessions are usually weekly or fortnightly in the early stages.
A patient’s history is taken regarding their past life experiences and background in the first session. Goal setting is an important part of the therapy from the outset. The ultimate goal is for you to become proactive in your own recovery.
How effective is C.B.T?
C.B.T. is believed to be one of the most effective treatments where anxiety or depression is the main problem. It is the most effective psychological treatment for moderate and severe depression. It is as effective as anti-depressants for many types of depression. However, for severe depression, CBT should be used with anti-depressant medication. When you are very low as I mentioned earlier it may be hard to change your thought process until anti-depressants have started to make you feel better.
Carr (2006) notes that the relapse rates for people who have received both medication and CBT is between (20-35%) as oppose to (50-80%) for those on medication alone during follow up studies.
Given the robustness of the CBT approach it seems clear that CBT needs to be part of the treatment approach to tackle depression.
References
- Greenberger D, Padesky C ‘Mind over Mood’ – Change how you feel by changing the way you think N.Y. Guilford Press, 1995.
- Beck A.T. Cognitive therapy and the emotional disorders N.York: International Universities Press, 1976.
- Seligman M.E.P. (2002). ‘How Psychology lost its way and I found mine’ in Seligman M.E.P. (ed) Authentic happiness Nicholas Brealey.
- Carr, C. and McNulty M (2006) ‘Depression in Carr, C and McNulty. M. (ed) The Handbook of Adult Clinical Psychology, Routledge.
- Segnl Z, Williams M and Teasdale J (2002) cited in Carr C and McNulty M The Handbook of Adult Clinical Psychology Routledge.
- Ellis A (1987) Cited in Walen, S.R. DiGiuseppe, R and Dryden, S. A Practitioners Guide to Rational Emotive Therapy, Oxford.
- Moore-Groarke, Distorted Thinking in CBT, A psychological perspective –‘Cognitive behavioural therapy for chronic pain’, Irish Psychiatrist, Sept. 2005.
- Moore-Groarke G, (2008) ‘In search of thinness’, Currach Press.
Useful online CBT resource
- Mood Gymn: http://Moodgym.anu.edu.au Information, quizzes, games, and skills training to help prevent depression.
